Houston Diabetic Foot Treatment
Foot and ankle health is key to maintaining overall health and well being. Having a healthy foot and ankle helps to maintain the integrity of the musculoskeletal system – which is key to maintaining quality of life. Mobility is essential for longevity.
Diabetic Foot Quick Facts
- Diabetic foot ulcers are responsible for more hospitalizations than any other complication of diabetes.
- These Ulcerations can have potentially devastating complications – causing up to 90% of lower extremity amputations in patients with diabetes.
- Peripheral neuropathy (PN) is present in 60% of patients with diabetes and 80% of patients with diabetes who have foot ulcers (resulting in a 12-27% lower limb amputation rate).
- There are nearly 80,000 diabetes related amputations each year – and a five-year risk of a contralateral amputation of 50%.
- The presence of a below the knee prosthesis requires a 25% increase in cardiac output for ambulation. Few diabetics have that level of reserve.
- The five-year mortality rate following below the knee amputation is 66% – usually from cardiac related issues.
Reference: OrthopaedicsOne, Diabetic Foot
The foot and ankle can also provide early indication of potential health problems or predisposition to later musculoskeletal conditions. Identifying these early signs will allow the correction of such conditions before they result in more serious limb…and life threatening problems. The diabetic foot is of particular concern and can be, if not closely monitored, instrumental in diminished health and longevity.
Foot ulcers are the most common medical complications of patients with diabetes, with an estimated prevalence of 12-15% among all individuals with diabetes (1). The prevalence of diabetic foot ulcers and their limb-threatening impact on the lower extremity stems from the decreased healing potential of a diabetic foot. This includes:
- Level of uncontrolled hyperglycemia
- Reduced circulation / arterial blood flow
- Inadequate nutrition
- Inability to offload the affected region of the foot
- Presence of infection
The diminished sensation associated with peripheral neuropathy (nerve damage present in 80% of foot ulcer patients with diabetes, causing weakness and numbness), increases risk of neglected injuries and fractures. This begins as overloading of the skin, which eventually leads to severe ulceration that fails to heal. Progressive weakening, much of which goes unnoticed as numbness often masks the extent of the problem, results in progressive weakening and degeneration of the limb.
While vascular studies are critical in determining the healing potential of foot ulcers and the need for surgical intervention, early assessment of other seemingly less serious conditions and limitations in foot conditions can prevent advancement to a more sever medical condition.
Early Signs of Concern
 Fortunately, there are a number of early warning signs indicating who is predisposed to potentially serious diabetic foot conditions. These early warning signs can also be an early indicator of other musculoskeletal imbalances before more serious problems result.
Fortunately, there are a number of early warning signs indicating who is predisposed to potentially serious diabetic foot conditions. These early warning signs can also be an early indicator of other musculoskeletal imbalances before more serious problems result.
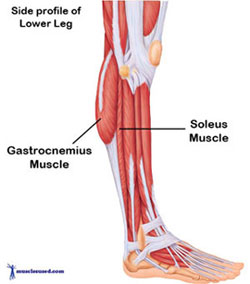
One of the most compelling warning signs and among the easiest to assess is the presence of a gastrocnemius/triceps surae contracture (tightening of Gastrocnemius muscle inhibiting normal dorsiflexion). This condition is increasingly associated with chronic foot conditions – and is proving to be an important preventive component for patients prone to conditions associated with the diabetic foot. It is also presented as a predisposing factor to such common foot conditions as metatarsalgia, forefoot ulceration, hallux valgus flatfoot deformity, Achilles tendinitis, plantar fasciitis, and Charcot arthropathy.
Preventive Treatment
When a patient shows an inability to dorsiflex through the tibiotalar joint with the heel in neutral or supination (at least 20 degrees of ankle dorsiflexion), a diagnosis of gastrocnemius and/or soleus contracture can be made. indicated to correct the contracture and restore balance of load on the foot. Distributing the load reduces risk of other chronic foot conditions, including diabetic ulcers.
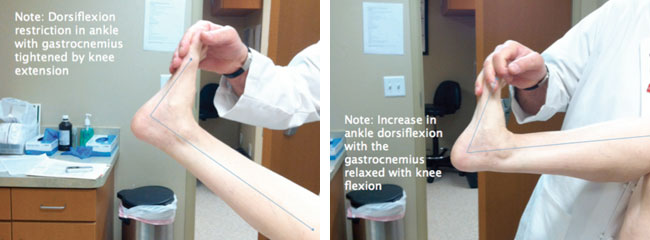
Total Contact Casting (TCC) may also be employed to offload plantar ulcers, which show signs of wound care failure. Once confirmed, a gastrocnemius +/- soleus recession is indicated to correct and restore balance of load on the foot. Distributing the load reduces risk of other chronic foot conditions such as diabetic ulcers. TCC may also be employed to offload plantar ulcers showing signs of wound care failure.
Life and Limb Saving Procedures for Diabetic Foot at the Sanders Clinic in Houston
The primary goal is to take early steps to reduce risks for potentially severe, limb threatening diabetic foot conditions. Effectively addressing advanced cases is critical for quality of life. Specialized procedures include deformity corrections, accomplished via a step-wise approach consisting of, but not limited to, soft tissue and tendon lengthening or release, occasionally followed by osteotomy, arthrodesis, or total ankle replacement, and/or tendon transfer.
References
American Diabetes Association: Diabetes statistics. www.diabetes.org/diabetes-basics/statistics
Pinney, SJ; Sangeorzan, BJ; Hansen, ST: Surgical anatomy of the gastrocnemius recession (Strayer procedure). Foot Ankle Int. 2004, 25(4):247-50.
DiGiovanni, CW; Kuo, R; Price, R; Cziernecki, J; Hansen, ST; Sangerorzan, BJ:
Clinical exam versus instrumented measurement of equinus in patients with fore foot pain. AOFAS Annual Summer Meeting, Vail, CO. 2000.
Hansen, ST: Functional reconstruction of the foot and ankle, Philadelphia, Lip pincott Williams & Wilkins, 2000.
Metatarsalgia
Known as a common “overuse” or “repetitive stress” condition affecting athletes, Metatarsalgia causes inflammation in the ball of the foot and is believed to be a symptom of other conditions, rather than a specific disease.
The primary symptom of metatarsalgia is pain located at the end of one or more of the metatarsal bones, which is aggravated when walking or running. Some athletes, who are involved in high-impact activities and may also suffer from an inflammatory condition such as bursitis, often have diffuse forefoot and midfoot pain.
The pain generally intensifies over time as opposed to resulting suddenly.
Forefoot Ulceration
Diabetic forefoot ulcers most often result from the combination of neuropathy and abnormal mechanical stress. Other musculoskeletal deformity may increase stress on a portion of the foot, promoting ulceration in a patient with diabetic neuropathy.
High forefoot pressure is consistent with the most common locations of foot ulcers – generally the plantar surface of the metatarsal heads and the hallux.
If not properly managed, foot ulcers can cause deep spreading infection and result in leg amputation. The prevention and cure of foot ulcers should prevent most leg amputations in patients with diabetes. The combination of neuropathy and decreased ankle dorsiflexion has been implicated in the cause of forefoot ulcers.
1.) Birke JA, Patout CA Jr, Foto JG. Factors associated with ulceration and amputation in the neuropathic foot. J Orthop Sports Phys Ther. 2000;30(2):91-97.
2.) Daniels TR. Diabetic foot ulcerations: an overview. Ost Wound Manage. 1998;44(9):76-84.
(Sources include: Medscape, http://www.medscape.com/viewarticle/505640)
Plantar Faciitis
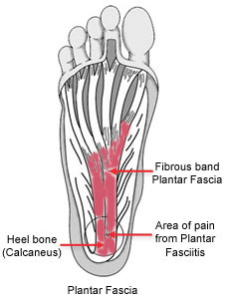 Plantar fasciitis is one of the most common causes of heel pain. Approximately two million patients are treated for this condition every year.
Plantar fasciitis is one of the most common causes of heel pain. Approximately two million patients are treated for this condition every year.
Occurring when the strong fibrous band of tissue (Plantar Fascia), which supports the arch of the foot, becomes irritated and inflamed, plantar fasciitis often develops without a specific reason or cause. There are, however, a number of factors that may predispose a person to the condition, including:
- Tighter calf muscles that make it difficult to flex the foot and bring toes up towards the shin
- Obesity
- Very high arch
- Repetitive impact activity (running/sports)
- New or increased activity
(Sources include: The American Academy of Orthopaedic Surgeons, AAOS.)
Charcot Arthropathy
 Charcot arthropathy, also known as Charcot foot and ankle, is a condition that can develop in patients who have neuropathy or loss of sensation, such as a diabetic patient. Early symptoms may include swelling and redness, which may progress and also include fractures and dislocations of bones and joints – that occur with minimal or no known trauma.
Charcot arthropathy, also known as Charcot foot and ankle, is a condition that can develop in patients who have neuropathy or loss of sensation, such as a diabetic patient. Early symptoms may include swelling and redness, which may progress and also include fractures and dislocations of bones and joints – that occur with minimal or no known trauma.
Diabetic patients experience damaged blood vessels, which decrease the blood flow to the feet. Poor circulation weakens bone and can cause disintegration of the bones and joints in the foot and ankle – often breaking bones in the feet.
Diabetic foot fractures also often present as more serious fractures, as the nerve damage diabetic patients experience often delays detection. Patients continue to walk on the injured foot – resulting in more severe fractures and joint dislocations. Broken bone edges can point downward toward the ground, increasing the risk of chronic foot sores from the abnormal pressure.
This combination of bone disintegration and trauma warping and deforming the shape of the foot is characteristic of Charcot arthropathy – and is one of the most serious foot problems that diabetics face.
